|
|
|
|
|
|
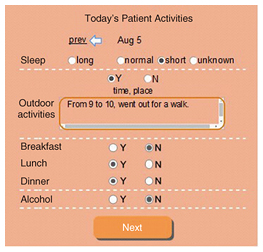
Feature Articles: Basic Research Envisioning Future Communication Vol. 14, No. 11, pp. 43–49, Nov. 2016. https://doi.org/10.53829/ntr201611fa7 How Tracking Technologies Improve Family CommunicationAbstractIn this article, we explore how health-tracking technologies could be designed to support family caregivers to better cope with the unexpected behaviors of a depressed family member. We designed a tracking tool called Family Mood and Care Tracker (FMCT) and deployed it for 6 weeks in the homes of 14 family caregivers looking after depressed family members. FMCT is a web-based tracking tool designed specifically for family caregivers to allow them to record their caregiving activities and the sufferers’ health conditions. Our findings demonstrate how the family caregivers made use of FMCT to better cope with depressed sufferers and how it improved the communication between family caregivers and sufferers. Keywords: depression, family caregivers, tracking technology 1. IntroductionThe onset of mental illness in a family places a significant burden on its members and causes a great deal of stress. In most cases, mental illness—as well as its medication—causes unexpected behaviors in the sufferer. For example, sufferers may become demanding and disruptive, or they might express extremely negative attitudes or excessive anger. When family caregivers face such circumstances, they often become puzzled and do not know how to react. In addition to the difficulty of coping with such unexpected behaviors, social stigma is attached to such illnesses, making it difficult for family caregivers to consult with others. Under such circumstances, most family caregivers tend to gather information about the illness themselves, although finding useful information is complicated due to the huge individual differences among symptoms. Consequently, family caregivers generally have little choice but to rely on discoveries based on their own experiences. Despite the significant impact of mental illness on families, much of human computer interaction and computer-supported cooperative work on mental illness has focused on either the patient or the clinician, aiming for better patient care. Little research has focused on supporting family caregivers. Our goal is to design new technologies that help family caregivers develop strategies to better interact with sufferers. In this article, we focus on computer diary based tracking technology and explore its potential to aid family caregivers. For example, by recording and tracking the sufferer’s moods and caring activities, family caregivers may be able to analyze how their behavior affected the sufferer’s moods/symptoms and thus discover effective coping strategies. Such behavioral change in caregivers may lead to better sufferer-caregiver relationships and prevent an escalation in stress between the two. Meanwhile, previous research also warns that family caregivers’ use of tracking technologies to monitor sufferers’ health may create sufferer-caregiver conflicts caused by the sufferer’s perception of surveillance, that is, an uncomfortable feeling of being monitored. Since individuals suffering from mental illness tend to have a high perception of surveillance, we need to be aware of its risks and pay extra attention to how tracking technologies affect domestic relationships. We explore the following research questions in this article: (1) how tracking technology might assist family caregivers’ development of coping strategies, and (2) whether/how it affects the relationships between family caregivers and sufferers. We investigate these research questions by focusing on caregivers who look after family members diagnosed with depression. To answer these research questions, we first conducted a preliminary interview study with 14 family caregivers who were looking after a depressed family member. The aim of this study was to identify the basic design features (e.g., items family caregivers wish to track, family caregivers’ concerns of using tracking technologies at home) of our tracking tool. Based on the interview study, we developed a web-based tracking tool for recording data and deployed it with 14 family caregivers (not members of the preliminary interview study) of depressed family members. During the deployment study, the family caregivers recorded their caregiving activities and the sufferer’s behaviors/moods for six weeks. The focus of the deployment study was to investigate the impact of tracking technology on the family caregivers’ development of coping strategies and the relationships between family caregivers and sufferers. 2. Preliminary interview studyTo identify the ways in which tracking technologies could be designed to support family caregivers, we interviewed 14 family caregivers looking after a depressed family member. From the interviews, we identified the basic design requirements of our tracking tool. Much information was gleaned from the interviews, including different ways family caregivers currently handle their caregiving tasks, and how technology might assist them in caregiving. 2.1 Current practicesSome family caregivers mentioned that they kept a caregiving journal. However, none wrote on a daily or regular basis. Furthermore, they typically only wrote about negative events such as arguments they had had with the sufferer, and they described their own feelings about those events as a way to let off steam. Although they sometimes reviewed their journal, they felt it discouraging and unhelpful because it was filled with negative and emotional descriptions. According to the family caregivers, some sufferers also kept a diary about their health conditions as part of therapy or treatment suggested by their doctors. However, most of the family caregivers mentioned that they avoided reading what the sufferers wrote due to privacy concerns. 2.2 Items to recordWhen family caregivers were asked what items they wanted to track, they listed a range of things that could be consequential to sufferer moods: weather, medication, amount of sleep, outdoor activities, meals, drinking (i.e., consumption of alcohol), their own caregiving activities, and unexpected events such as phone calls from a friend or fighting and/or arguments. For example, many mentioned that the sufferer’s mood became worse when it was rainy or when the atmospheric pressure decreased. They also mentioned that sufferers either ate too much or did not eat at all when they were in a bad mood. Some seemed to notice a change in sufferer behavior after a change in medication. The articulation of unexpected events was expected to help them better understand the disease. 2.3 Concerns about using tracking technologies at homeAlthough many participants showed interest in detecting the signs of mood changes in the sufferers or in developing coping strategies to achieve more positive interactions with them, they also expressed some concerns about using tracking technologies at home. Many worried that sufferers might perceive surveillance by having their details recorded. They also worried that sufferers might accidentally read the recordings and take them negatively. Overall, the family caregivers were concerned that tracking the sufferer’s mood/behavior might cause sufferer-caregiver conflicts. Finally, the family caregivers worried about the additional workload caused by using the technology. 2.4 Technology requirementsThe current practices suggest that our tracking tool should: • promote unbiased recording (i.e., not just negative events) in order to support positive self-reflection by the family caregivers. • not take advantage of recorded data of sufferers, meaning that data input will be done solely by family caregivers. • include the following items: weather, medication, amount of sleep, outdoor activities, consumption of meals and alcohol, their own caregiving activities, and unexpected events. • work not only on ordinary personal computers but also on mobile devices to support family caregivers’ private data input. • minimize the burden of data input. 3. Tracking tool designThe Family Mood and Care Tracker (FMCT) tracking tool consists of two sections: recording and reviewing. The recording section allows the family caregivers to record data, and the reviewing section facilitates reflective analysis by family caregivers through visualization of the recorded data in a chart. 3.1 Recording sectionThe recording section allows the family caregivers to record all of the items identified in the preliminary interview study: the sufferer’s mood, medication, amount of sleep, outdoor activities, consumption of meals and alcohol, their own caregiving activities, and unexpected events. One of the pages of the recording section is shown in Fig. 1. To minimize family caregivers’ input burden, most recording items consist of multiple-choice questions. For example, for the sufferer’s sleeping, the caregivers enter the amount of sleep by selecting from four choices: long, normal, short, and unknown. The weather information (atmospheric pressure, highest/lowest temperatures, and actual weather conditions) was automatically retrieved from a weather information site.
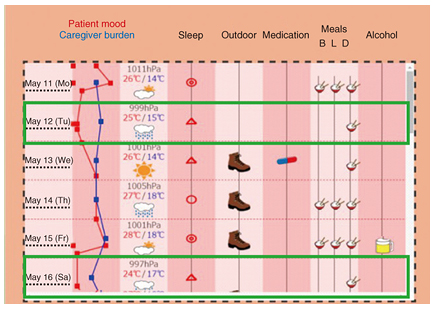
Free-form text boxes were provided for three items: outdoor activities, own caregiving activities, and unexpected events. For outdoor activities, the caregiver could enter details of where the sufferer went and for how long. For own caregiving activities, three free-form text boxes were prepared. Each box prompted input on positive and negative outcomes of their caregiving activities as well as lessons learned. We expected these three items to facilitate caregivers’ unbiased reflection on their daily caregiving activities and help them develop coping strategies for the future. Finally, a free-form text box was prepared to facilitate reflection prompted by unexpected events. Since unexpected events happen on an irregular basis, the data input to this field was optional. 3.2 Reviewing sectionThe reviewing section displays a chart that facilitates the caregiver’s reflection on his/her caregiving activities and the sufferer’s conditions (Fig. 2). All of the data were displayed in a single chart so that caregivers could explore their data in a holistic manner. The chart shows the sufferer’s mood (red line) and caregiver burden (blue line) as graphed lines; the closer to the left a graph point is, the more negative it is. Weather information and other data are shown as icons.
Family caregivers can also see the unexpected events and the caregiving activities recorded on a particular day by clicking on a date, which makes a textbox pop up that shows the recorded data. Another textbox for the details of outdoor activities also pops up by clicking on the shoe icon. We expected this chart to help family caregivers identify the sufferer’s health condition patterns and develop coping strategies. From Fig. 2, for example, we see that the sufferer tends to stay indoors or skip breakfast/lunch when he is in a bad mood (as highlighted in green boxes). 4. Deployment studyWe conducted a six-week deployment study with FMCT to investigate how family caregivers’ tracking behaviors affected their caregiving activities and interaction with sufferers. The study was reviewed and approved by the ethics committee of NTT (ethics review ID: H27-011). 4.1 Participants: family caregiversWe recruited 15 family caregivers (12 females and 3 males, mean age = 43.0) for the deployment study from the same consumer marketing company used for the preliminary interview study. In the recruiting process, any family caregivers who were themselves diagnosed with major depression were excluded. Thus, we ended up with 14 family caregivers, as mentioned above, who were currently looking after a depressed family member. Nine caregivers were spouses of sufferers, two were parents, two were daughters, and one was a sibling. All of the caregivers lived with the sufferer and held primary responsibility for looking after them. Six caregivers were full-time homemakers, six had full-time jobs outside the home, and two worked at home. 4.2 ResultsAlthough this study was meant to be the first step to reach our goal (i.e., to develop new technologies for better patient-caregiver relationships), our tracking also received a surprisingly high evaluation from the family caregivers. Indeed, most participants (12) noted in the interview that they became more actively engaged in the care, gained better control over the sufferer’s moods, and increased/improved communication with the sufferers. Below, we analyze how such changes were made through the data obtained by FMCT. 5. Interview findingsWe report here some of the caregivers’ views and comments on the use of FMCT to support their caregiving activities. 5.1 Becoming attentive to sufferer’s behaviorsIn general, the survey results showed that family caregivers perceived themselves as becoming more attentive to the sufferer’s behaviors (mean (M) = 1.93, standard deviation (SD) = 0.65 on a 5-point Likert scale: 1 = became very attentive, 5 = did not become attentive at all). One participant described how using FMCT produced greater attentiveness toward her sufferer’s moods and behaviors: [Identification (ID) 7, full-time employee, daughter of sufferer] “Since I’m always busy in the morning, I didn’t really care if she was in a good or bad mood. But after I started to use this [FMCT], I paid more attention to her condition to find something to record. Like her mood while eating breakfast and her tone of voice.” Another participant, whose husband experienced a relapse two years ago, mentioned that she started to pay extra attention to his medication: [ID 1, homemaker, wife of sufferer] “I feel like I’m now more involved with my husband’s illness. I started to watch him more carefully, and I realized that he often forgot to take some of his medication.” Accordingly, although the family caregivers’ access to FMCT was limited (1.52 times per day), the recording items seemed to remind them of the things to which they should pay attention when they were with the sufferers. Consequently, most family caregivers became more attentive to their sufferer’s behavior, and such attentiveness led them to new findings about the sufferer’s behaviors. 5.2 Making better sense of sufferer’s behaviorBy becoming more attentive to sufferer moods and behaviors, family caregivers noticed subtle things that they never noticed before. These details seemed to provide cues to better understand mood changes and behavioral patterns. For example, one participant realized that her mother’s mood was greatly affected by the weather: [ID 2, full-time employee, daughter of sufferer] “I wasn’t even aware that weather affected my mother’s mood. During the study, I realized a couple of times that when she was out of sorts, the weather was also bad.” As with ID 2, many family caregivers realized that there are underlying reasons for the mood changes of sufferers. Although our study gathered no concrete evidence that their individual discoveries were true, the family caregivers seemed to feel that they could make better sense of the sufferer’s behaviors by recording and reviewing the sufferer’s moods and activities every day. 5.3 Developing concrete action plansSuch discoveries of sufferer moods/behaviors affected the family caregivers in multiple ways. For example, the discoveries helped them develop concrete action plans to effectively support the sufferers. In other words, the family caregivers gained a clearer sense of what they should and should not do/say to the sufferers. ID 1, whose husband often forgot to take his medicine, described how she came to provide help: [ID 1, homemaker, wife of sufferer] “I talked to my husband when I noticed that he hadn’t taken all of his medication. I thought he knew, but to my surprise, he didn’t. Since he is a well-organized person, I had been assuming that he could manage by himself. But I realized that there were certain things that he couldn’t manage. I decided to support him in these areas.” Other family caregivers reviewed the FMCT graph and searched for clues to better cope with their sufferers. For example, one family caregiver described how she successfully handled her mother’s unexpected behavior by reviewing the FMCT record: [ID 7, full-time employee, daughter of sufferer] “My mother was in a good mood while eating supper, but she suddenly got very quiet. I wondered why and reviewed the [FMCT] record. While tracking back, I started to wonder what things made her happy. Then I found a case where my mom became happy when I praised her cooking. I instantly thought this might be the case. I realized that in this case, I had just eaten silently without praising her cooking. I went to her and said, “Your cooking was so delicious that I completely forgot to thank you.” I was relieved to see her returning to normal.” As with ID 7, some caregivers reviewed the FMCT record when things went wrong, developed a hypothesis and an action plan to improve the situation, and tested it on the sufferers. Again, we do not know if ID 7’s hypothesis was correct—the sufferer may have had different reasons for her change in mood. However, the important point is that FMCT appeared to be useful from the family caregiver’s perspective (ID 7 in the case above). Through building and testing hypotheses, family caregivers seemed to realize that there are some connections between their own behavior and the sufferer’s mood/behavior. Some family caregivers even noticed patterns between the two: [ID 4, full-time employee, husband of sufferer] “Previously, I couldn’t understand why her mood went down. Although I had a feeling that I had said something wrong, it quickly faded from my memory. By tracking and reviewing every day, I detected certain patterns. Similar things happened over and over. I knew that praising was good in my head, but I came to realize how important it is to praise her as a real experience.” Such discoveries seemed to help the family caregivers realize that there are certain things they, as family caregivers, could do to improve the current situation. According to the family caregivers, the lessons learned section was particularly useful for keeping track of the trial-and-error results of their hypotheses and for developing better coping strategies. The holistic view of sufferer mood and caregiving activities also seemed to help them analyze the connection between the two, and to think of a new coping strategy. Throughout the process, many family caregivers seemed to perceive themselves as becoming attentive to their own behaviors (M = 2.28, SD = 0.78 on a 5-point Likert scale: 1 = became very attentive, 5 = did not become attentive at all). 5.4 Changing views on sufferersThe family caregivers’ discoveries about sufferer moods/behaviors also seemed to affect their views on the sufferers. Many realized that their views were biased or unfair. For example, one family caregiver who had experienced depression himself described how he came to realize that giving his daughter advice based on his own experience could be inappropriate: [ID 10, working at home, father of sufferer] “I recently realized that my daughter’s experience of depression might be different from mine. Hers is seasonal, but mine isn’t. I knew this for a fact, but I actually didn’t understand the difference. (…) I tended to give her advice based on my own experience. I guess I was being over-possessive at times. (…) While reviewing the graphs, I noticed a correlation between the weather and her moods, and I started to feel that her depression might be totally different from mine.” As with ID 10, by reviewing the FMCT records, some family caregivers realized that their views had been unfair. Some also mentioned that their views about the sufferers gradually changed as they entered the positive outcomes field of their caregiving activities every day: [ID 11, full-time employee, wife of sufferer] “I realized that he himself is making an effort. For example, one day when he went to the library, he borrowed a book for me because he thought I might like it. By keeping records, I realized how much he cares about me, the small things that I would normally pay no attention to. (…) I used to think that it was always me, the caregiver, who provides support, but after using this tool, I felt as if we could care for each other.” Overall, the recording items of FMCT (particularly filling out the positive outcomes field) seemed to facilitate positive self-reflection on the family caregivers’ caregiving activities. It provided them a chance to reconsider their caregiving habits and objectively think about how they had been communicating with the sufferers. As a result, many family caregivers realized that their views on sufferers had been biased, which helped them mitigate their biased thoughts of the sufferers. 5.5 Being generous to sufferersSuch changes in the family caregivers’ views affected their attitude toward the sufferers. Aside from some specific coping strategies to deal with unexpected sufferer behaviors, many family caregivers mentioned that they became more generous to them: [ID 10, working at home, father of sufferer] “I don’t think this [FMCT] tool is critical, but it does have its uses. It changed the way I communicate with my daughter. I used to brush her off and criticize her opinions. But I started to feel that I should be more generous and listen to her until she was finished without criticizing her, even when I think she’s wrong.” [ID 11, full-time employee, wife of sufferer] “I can now see that the disease is the troublemaker, not him. (…) I started to avoid saying negative things to him. Consequently, FMCT seemed to give family caregivers breathing room to take a step back and communicate with the sufferers in a more relaxed manner.” 5.6 Achieving better communication with sufferersFinally and most importantly, although we were concerned that family caregivers’ use of FMCT might create patient-caregiver conflicts, none of the family caregivers reported such an effect. In fact, most reported the opposite: [ID 2, full-time employee, daughter of sufferer] “The amount of communication with my mom definitely increased. Previously, communication often started with a complaint, for example, “Why did you do this or that?”, and so our communication tended to be antagonistic. (…) During this study, I had to ask her some questions to record her daily activities. After I returned from work, I asked her about her day, whether she had eaten lunch, how she was feeling, etc. There was no reason to become antagonistic about these questions. They can be asked in a normal tone. My mom also looked pleased when I asked them. I think she felt cared for.” Some even reported that the sufferers became more proactive when talking about their health conditions: [ID 3, homemaker, wife of sufferer] “To record his condition, I often asked him some questions such as whether he had slept well last night and so on. Gradually, he started to talk about his condition before I asked him. (…) Previously, it was comments like “I’m tired” or “I’m exhausted,” and nothing else. But he’s started to elaborate on his condition and show that he is thinking about the future. (…) I felt like he was indirectly participating in the study. It’s good to have a common goal and to collaborate in keeping the record and fighting the disease.” As with IDs 2 and 3, although family caregivers initially asked questions of the sufferers (e.g., whether they had eaten lunch or not) to maintain the FMCT records, those questions seemed to please the sufferers and open up thoughtful communication between the sufferers and the family caregivers. Overall, the recording items seemed to serve as a spring board to start a safe conversation with the sufferers. Together with the family caregivers’ relaxed attitudes, such conversation led them to a positive communication cycle. 6. ConclusionThis article explained the potential of tracking technologies to support family caregivers in interacting more effectively with sufferers of depression. Our findings are significant in three ways. First, the manual input of sufferer mood/behavior by family caregivers promoted higher attentiveness to the sufferers and helped them understand the sufferer better. Second, the selected recording items and the holistic view of sufferer mood/behavior and caregiving activities helped the family caregivers develop effective coping strategies. Third, the recording items served as a spring board to initiate a safe conversation with the sufferers. Altogether, our technology probe changed the ecology of the family caregivers, sufferers, and the disease from sufferer with disease vs. family caregiver to sufferer and family caregiver vs. disease. We believe our study will open up new ways of using tracking technologies in the field of mental healthcare. |
|